At Neuroelectrics, we believe in the advantages and effectiveness of transcranial electric stimulation (tES) in treating numerous brain diseases. Yet, despite the increasing number of tES publications per year, the lion’s share in the market of non-invasive brain stimulation technologies is still played by transcranial magnetic stimulation (TMS), likely because TMS received US-FDA approval in 2008 whereas tES has not yet.
Does this mean TMS is more effective? Well, it’s not quite fair to say so, considering TMS studies started at least 10 years earlier than those of tES. Therefore, there are several more clinical trials proving TMS efficacy.
However, the two techniques are close relatives: you can think of TMS as the elderly, stiff and sturdy brother, and tES as the younger, more flexible and easy-going one.
In this blogpost, we’ll go over the roots of their differences and see when and why you might prefer one over the other.
[E-fields patterns and biophysical substrates]
At a fundamental level, the two techniques rely on different physics and induce distinct patterns of electric fields (E-field) on the cortex, acting on a different neural substrate.
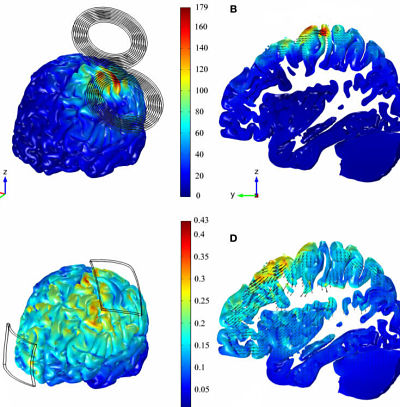
TMS is based on electromagnetic induction: a large magnetic coil is placed just a few centimetres above the scalp to stimulate over a specific cortical area. When the operator launches the electric pulse, vast amounts of current flows suddenly through the coil and creates a magnetic field around it, which varies rapidly in time. This changing magnetic field induces a very short (order of 1ms), highly localized (figure 1), super-threshold (order of 100V/m) E-field in the cortex. The E-field maximum is reached on the gyrus right under the coil, and the orientation is mostly parallel to the cortical surface.
The most sensitive cells to an E-field with such characteristics are interneurons and collaterals of pyramidal cells aligned tangentially to the cortical surface, which are automatically triggered to fire.
Instead, tES operates in the (quasi-)static regime, as only a small amount of direct current (DC) or low frequency alternating current (AC) is applied through electrodes placed directly on the scalp. The temporal resolution of the technique is low because the neuromodulatory effects begins a few seconds after the start of stimulation. Moreover, the E-field generated is much weaker (order of 0.1V/m) and less focalized (although the focality can be improved by using multichannel montages, it remains much lower than TMS E-field). Depending on the electrodes’ geometry, the maxima can occur on the gyri at the edges of the electrodes or between them. The overall orientation of the E-field is normal to the cortical surface, which indicates that tES probably influences layer V pyramidal neurons, as they are mostly perpendicular to the cortex.
Given the low, subthreshold intensity, the tES E-field cannot cause neural firing, but it is able to modulate the firing rate, facilitating or inhibiting the activation of pyramidal cells.
[Devices]
Other important differences concerning system setup.
TMS technology is more complex and cumbersome. The cost of the whole equipment is between 50-100k USD or Euros. This includes a wall-powered and heavy stimulator about the size of a fridge, a coil connected to the stimulator by a high-voltage cable, a mechanical arm to hold it in place, and a neuro-navigation system to accurately place the coil over the target brain region. The coil hangs suspended over the head of the patient, and since the strength of the effects depends on the coil-cortex distance, it’s crucial to keep it at the specific distance. For this, during the treatment session, the patient must sit still in a specially designed chair, with positioning frames around the chin and forehead.
On the contrary, tES is much cheaper and effortless: the cost is between an average of 6-30k USD/Euros, and the whole setup fits a shoe box. The stimulator can be as small as a mobile phone, light/portable, and almost always battery powered. The electrodes are directly in contact with the scalp, held in place by a rubber band or a neoprene cap. This way, the patient can move and even walk during the stimulation session.
[Applications]
Despite the underlying differences, TMS and tES are both quite versatile tools for treatment and research, and they offer similar options.
In research settings, you can leverage on TMS’ high spatial and temporal resolution to study how brain networks dynamically operate. In this context, TMS is usually performed online (during task performance) by applying one pulse at the onset of a stimulus (single-pulse TMS), or two pulses over separate regions which are interconnected (paired-pulses TMS). But tES too allows one to study the causal link between cortical areas. For instance, with tACS, one can simultaneously apply oscillatory currents over distinct regions at the same frequency but with different phases to promote or hamper the synchronization of functional networks.
Clinical applications of brain stimulation techniques instead tend to focus more on long-term effects, promoting network neuroplasticity that can outlast the period of stimulation.
In this case, TMS is usually ran in the repetitive mode (rTMS), which consists in multiple pulses within just microseconds. Frequency lower than 1Hz has been linked to long term depression (LTD), whereas frequency above 5Hz to long term potentiation (LTP). Similar outcomes can be achieved with tCS using either tDCS anodal or cathodal stimulation, which has been shown promoting and inhibiting synaptic activation, respectively.
The side effects of both techniques are quite moderate – with one important exception. While tES can induce only mild and temporary itching, tingling, and skin reddening when done properly, TMS might cause mild headaches, facial twitching, seizures in extreme cases.
For both TMS and tES, medical treatment must be performed mostly in clinical settings, which means you will have to find a clinician who provides these services in their clinic. However, one of the strengths of tES is the possibility to perform stimulation telemedically (under the remote guidance of a clinicians) via home-treatment. This is important as it will boost therapeutic effects for pathologies such as motor rehabilitation, depression, Alzheimer’s disease, etc in the comfort of one’s home. And it has been shown that the number of sessions modulates the length of the long-term plastic effects.
Interested in home-application of tCS? Check our home-kit here.

[REFERENCES]
Polanía R, Nitsche M.A., Ruff C., Studying and modifying brain function with non-invasive brain stimulation, Nat. neurosci., 21:174–187 (2018)
Dayan E., Censor N., Buch E.R., Sandrini M, Cohen L.G., Noninvasive brain stimulation: from physiology to network dynamics and back, Nat. Neurosci., 16:838–844 (2013)
Salvador R., Wenger C., Miranda P.C. Investigating the cortical regions involved in MEP modulation in tDCS, Front. Cell. Neurosci. 9:405 (2015)
thebrainstimulator.net/brain-stimulation-comparison/caputron.com/pages/tms-vs-tdcs