We received in April this year a grant from the Michael J. Fox Foundation for Parkinson’s Research (www.michaeljfox.org), which is dedicated to finding a cure for Parkinson’s disease (PD). The idea of the grant is to study if advanced Machine Learning techniques can help in predicting the appearance of Parkinson’s. The grant runs for a year. I would like to report today on our progress in this research.
Background and data set
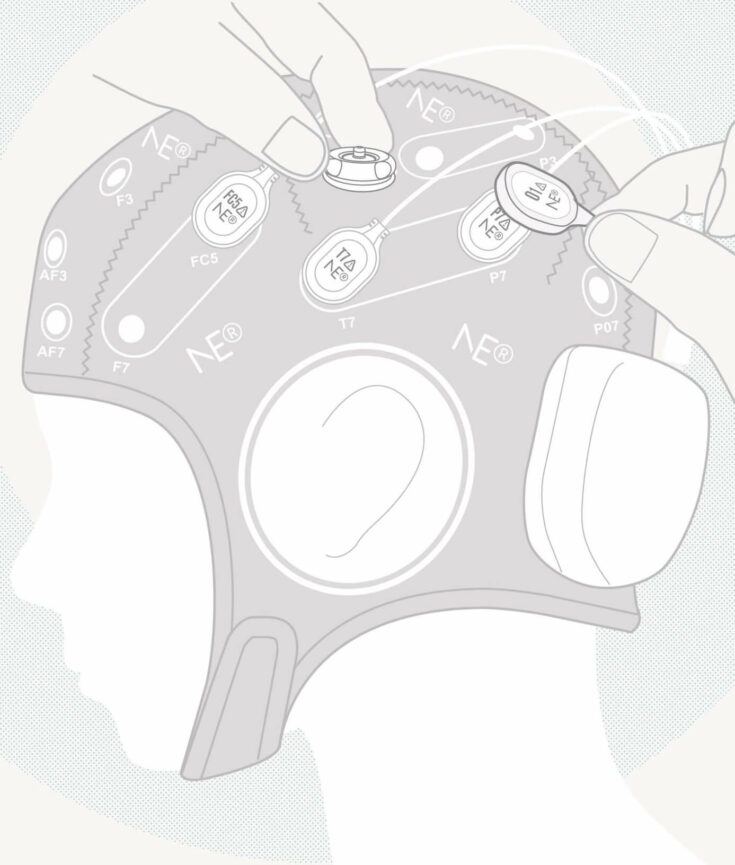
In the project we analyze EEG data acquired by the Center for Advanced Research in Sleep Medicine (CARSM)1 of Hôpital Sacré-Coeur de Montréal. The data was obtained from approximately 60 subjects suffering from REM Behaviour Disorder (RBD) and 60 healthy controls. RBD2 is a sleep disease whereby the subjects suffering it lose motor inhibition while dreaming. This makes them act out their dreams, which can present as aggressive behavior while sleeping. The interesting feature of that data is the fact that the EEG was acquired years before some of the subjects with RBD develop different neurodegenerative diseases like Parkinson’s.
The relationship between RBD and neurodegenerative diseases3 has been known for a while. Subjects with RBD develop, after 10-15 years on average, some neurodegenerative disease, namely approximately 30% of subjects develop Parkinson’s, 30% develop Lewy Body Dementia, 5% Multiple System Atrophy, 20% other diseases, whereas 15% remain having only RBD. Well this is not fully correct. New findings4 are showing that it is only a question of time before this 15% develop some type of neurodegenerative disease.
RBD patients have characteristic EEG
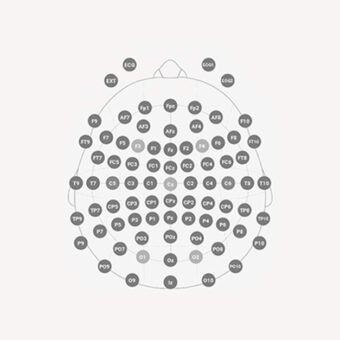
Several scientific papers have analyzed how EEG can be used to characterize RBD in this context. Differences have been found in the frontal, central, and occipital areas of the cortex. Particularly subjects suffering RBD present5 larger power in low frequencies than healthy subjects. For frequencies above 15 Hz this relation toggles, so that RBD subjects have less power in these bands than healthy subjects.
Another group go a bit further in his EEG analysis. They explained6 that those RBD patients that 2.5 years after the EEG acquisition would develop minimum cognitive impairment presented a characteristic EEG. Power in the low frequency bands was larger than those RBD patients who do not develop the cognitive impairment and also than the healthy subjects involved in the study.
What is Machine Learning good for?
The papers mentioned above claim therefore that EEG characteristics can be used as an indication (so-called biomarker) of RBD development. You are surely thinking the diagnostics problem is solved. But one piece is missing: Machine Learning. I explain why in the following.
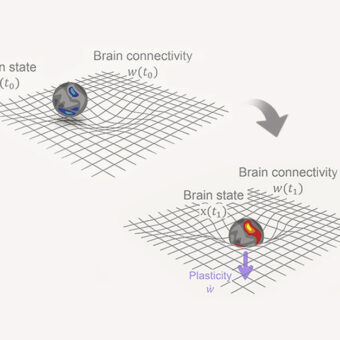
The papers previously cited ground their statement on group comparisons. This means: taken as a group RBD subjects have larger power in the frontal EEG electrodes than healthy subjects, again taken as a group. These papers state that there is a statistical significance in the difference between one group and the other. Diagnostic decisions are made on individuals, not on groups. So for this to happen you need a decision system where you input the data of a particular individual subject and get the answer whether this individual is likely to develop for instance a neurodegenerative disease. This is the function of classifiers (or if you prefer Machine Learning, Computational Intelligence).
So in our project we are designing such an early diagnostic system. We envisage we will input the EEG of a subject in our system and will try to predict if this subject is likely to develop Parkinson’s Disease 10-15 years in advance. So far we are obtaining excellent results in the evaluation of the classifiers we have developed. We are managing to predict individual RBD development with a large percentage of the 120 subjects we are analyzing. This make us confident we will be able to develop such an early diagnostic system, although there is yet some way to go. With this and so-called neuroprotection7 we hope to improve the future of Parkinson’s patients.